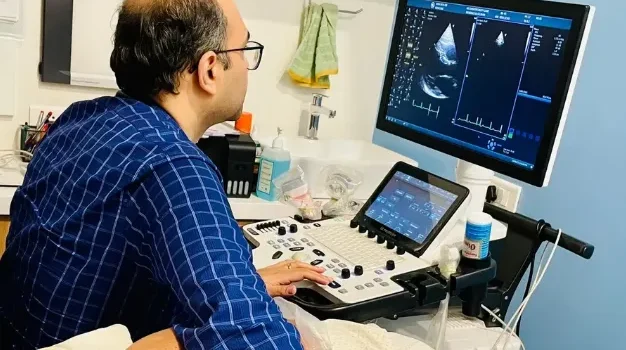
If you’re struggling with controlling your blood pressure, an echocardiogram might be a helpful tool to understand the impact high blood pressure may have already had on your heart. This non-invasive ultrasound procedure provides detailed images of the heart’s structure and function, offering crucial information to guide treatment and improve long-term blood pressure management.
When Might Your Doctor Suggest an Echocardiogram?
Healthcare professionals follow guidelines from established organizations like the American Heart Association (AHA) and the European Society of Cardiology (ESC) to manage high blood pressure (hypertension). These associations agree that echocardiograms play a key role in diagnosing and managing hypertension, especially in patients with hard-to-control blood pressure.
An echocardiogram may be recommended if:
- You show signs of heart damage possibly caused by prolonged high blood pressure. It can detect subtle changes that may be overlooked during routine physical exams.
- You have symptoms like shortness of breath, fatigue, or swelling in your legs and feet, which could indicate heart failure. The echocardiogram helps assess how hypertension has affected your heart’s pumping function.
- Your doctor wants more precision in evaluating your risk of future cardiovascular issues such as heart attacks or strokes. The test offers additional insights beyond standard risk assessments.
The Role of Echocardiograms in Blood Pressure Management
Echocardiograms provide essential information on how blood pressure affects your heart and help with better management of the condition. Here’s how:
Detecting Left Ventricular Hypertrophy (LVH)
The left ventricle, responsible for pumping blood throughout the body, can become enlarged and thickened due to chronic high blood pressure. This condition, known as left ventricular hypertrophy (LVH), is the heart’s way of coping with the added pressure. While it may seem like a compensatory mechanism, LVH increases the risk of heart failure and arrhythmias.
An echocardiogram can detect LVH earlier than other methods and help assess the extent of the thickening. By understanding the specific characteristics of the thickened tissue, doctors can determine the most appropriate treatment approach to prevent further damage and improve heart function.
Evaluating Systolic Function
Echocardiography also measures how effectively the left ventricle pumps blood, known as systolic function. Reduced systolic function can lead to symptoms such as fatigue, shortness of breath, and swelling, and increases the risk of heart disease even if blood pressure remains normal.
The test quantifies ejection fraction (EF), which indicates the percentage of blood the left ventricle pumps out with each beat. If your EF drops below 40%, it often signals the need for more specialized care. For borderline cases, advanced echocardiographic techniques like strain imaging can detect subtle dysfunction that might not appear on a standard test, prompting more aggressive treatment.
Assessing Diastolic Function
In addition to systolic function, the heart must also relax properly between beats to refill with blood—a process called diastolic function. Hypertension can cause the heart muscle to stiffen, impairing diastolic function and leading to blood buildup in the lungs, which results in shortness of breath.
Echocardiograms can assess diastolic function through various indicators, such as left atrial size and blood flow patterns across the heart valves. Advanced imaging techniques like tissue Doppler and deformation imaging offer further insights, allowing doctors to determine the most effective blood pressure targets. It’s important to strike a balance—blood pressure should be low enough to reverse LVH, but not so low that it interferes with proper diastolic filling.
Identifying Secondary Issues Linked to Hypertension
Hypertension affects more than just the heart—it can strain other parts of the cardiovascular system. Echocardiography helps detect complications such as:
- Pulmonary Hypertension: High blood pressure in the lungs can increase the workload on the right side of the heart and worsen heart failure symptoms.
- Left Atrial Enlargement: This can indicate ongoing high blood pressure and lead to an increased risk of stroke. The enlargement may also require regular rhythm monitoring.
- Aortic Dilation and Valve Abnormalities: Hypertension can accelerate the aging process of blood vessels, leading to aortic enlargement or valve issues. These conditions may require additional tests or even surgery to prevent life-threatening complications like aortic rupture or valve failure.
Conclusion
An echocardiogram is a powerful diagnostic tool in the management of high blood pressure. It not only helps identify damage caused by hypertension but also provides essential information to guide treatment decisions. Whether it’s detecting LVH, evaluating heart pumping function, or monitoring for other complications, an echocardiogram offers valuable insights that help protect your heart health over time.